Abstract
Introduction: Bridging radiotherapy (BRT) may be used prior to chimeric antigen receptor T-cell (CAR T) infusion for tumor cytoreduction, symptom palliation, and lymphodepletion. Case series on BRT are small and typically limited to single-institution reports. Herein, we report a multi-institutional analysis of the use of BRT prior to CD19-targeting CAR T therapy for relapsed/refractory B-cell lymphomas, with a focus on BRT characteristics, toxicity, and disease outcomes.
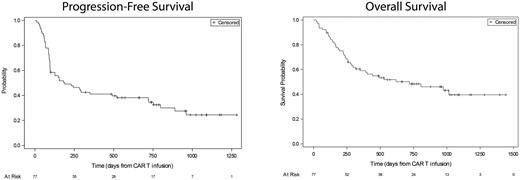
Methods: We retrospectively analyzed 77 patients with diffuse large B-cell lymphoma (n=64, 83%), primary mediastinal B-cell lymphoma (n=11, 14%), mantle cell lymphoma (n=1, 1%), and T-cell/histiocyte rich large B-cell lymphoma (n=1, 1%) who underwent CAR T therapy between 2018 and 2020 at 4 academic institutions. All received BRT within 1 month prior to leukapheresis up until CAR T infusion. BRT toxicities were graded with CTCAE v5.0, cytokine release syndrome (CRS) per ASTCT, and immune effector cell-associated neurotoxicity syndrome (ICANS) using either ASTCT or CTCAE v5.0. PET/CT response post-CAR T therapy was determined according to Lugano criteria. Patterns of failure were classified with respect to both BRT fields (in field, out of field, or both) and immediate pre-CAR T sites of disease (prior site, new site, or both). Progression-free survival (PFS) and overall survival (OS), measured from CAR T infusion, were estimated using the Kaplan-Meier method and modeled using Cox regression.
Results: Patients received axicabtagene ciloleucel (axi-cel; n=56, 73%), tisagenlecleucel (tisa-cel; n=20, 26%), and brexucabtagene autoleucel (n=1, 1%). Median age was 64 years (range, 24-81). Majority (n=41, 53%) were female and had advanced stage III/IV relapsed/refractory disease (n=60, 78%). ECOG performance status was 0/1/2/3 for 18 (24%), 41 (55%), 13 (17%), and 3 (4%), respectively. Median prior lines of therapy was 3 (range, 1-6). Extranodal disease was present in 49/75 (65%), central nervous system (CNS) involvement in 8 (10%), and bulky disease (lesion ≥7.5 cm) in 41/69 (59%). Systemic bridging therapy, excluding steroids, was given to 27 patients (35%).
Median interval from leukapheresis to BRT start and from BRT end to CAR T infusion were 7 days (interquartile range [IQR], 3-12) and 12 days (IQR, 9-17), respectively. 19 patients (25%) received BRT to more than one anatomic site. BRT was delivered to the abdomen/pelvis (n=39, 51%), head/neck (n=18, 23%), thorax (n=11, 14%), extremity/soft tissue (n=10, 13%), CNS (n=6, 8%), spine/paraspinal region (n=6, 8%), and axilla (n=6, 8%). Median BRT dose was 26 Gy (range, 4-45), median fraction dose 3 Gy (range, 1.3-15), and most common regimen 20 Gy in 5 fractions. 26 patients (34%) received BRT to all active lesions.
No grade ≥3 BRT toxicities were observed. Grade ≥3 CRS occurred in 5 patients (6%; 4 Grade 3 and 1 Grade 4). Grade ≥3 ICANS occurred in 17 patients (22%; 13 Grade 3 and 4 Grade 4), including 16/56 (29%) who received axi-cel and 1/20 (5%) who received tisa-cel. 25 patients (32%) received tocilizumab and 30 (39%) received steroids for CAR T toxicity.
At a median of 33 days (IQR, 29-66) to first restaging PET/CT, overall response rate (ORR) was 83% (complete response 37/75, partial response 25/75). At a median follow up of 31.3 months (95% CI, 24.3 - 33.6), 44 patients (57%) had experienced disease progression and 41 (53%) had died. Patterns of failure were detailed for 41 patients and included within the BRT field only (n=4, 10%,) out of field only (n=25, 61%), and both (n=12, 29%). Failure occurred at immediate pre-CAR T sites only (n=5, 12%), new sites only (n=15, 37%) and both (n=21, 51%). 1- and 2-year OS rates were 59% and 48%. 1- and 2-year PFS rates were 41% and 35% (Figure 1). On multivariable analysis, age ≥65 (hazard ratio [HR] 1.9, p=0.040), CNS involvement (HR 4.5, p=0.0028), ≥3 prior lines of therapy (HR 2.1, p=0.0095), and bulky disease (HR 2.4, p=0.0063) were associated with inferior PFS.
Conclusions: In this multi-institutional study, patients receiving BRT frequently had bulky disease yet experienced favorable ORR, PFS, and OS after CAR T therapy. There were no serious BRT toxicities and acceptable rates of CAR T toxicity. Isolated failure within the BRT field alone was uncommon. Future studies are needed to better define patient selection criteria for BRT versus other bridging therapies, as well as clarify the utility of "debulking” BRT prior to CAR T therapy.
Disclosures
Sim:ViewRay, Inc.: Research Funding. Jain:Incyte: Research Funding; MyeloidTx: Consultancy; BMS: Consultancy; Novartis: Consultancy; Kite Pharma: Consultancy, Research Funding. Schuster:Morphosys: Consultancy; Merck: Research Funding; Genentech: Consultancy, Research Funding; DTRM: Research Funding; Adaptive Biotechnologies: Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Incyte: Consultancy, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Juno Therapeutics: Consultancy, Research Funding; BeiGene: Consultancy; Roche: Consultancy, Research Funding; AbbVie: Research Funding; Genmab: Consultancy; Fate Therapeutics: Consultancy; Loxo Oncology: Consultancy; Legend Biotech: Consultancy; Mustang Biotech: Consultancy; Pharmacyclics: Research Funding; AstraZeneca: Consultancy; TG Therapeutics: Research Funding; Nordic Nanovector: Consultancy; Regeneron: Consultancy; N/A: Patents & Royalties: Related to CD19 CAR T cells and autologous co-stimulated T cells. Chong:Juno/BMS: Consultancy; Tessa: Consultancy; KITE: Consultancy; Beigene: Consultancy; Novartis: Consultancy. Plastaras:Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal